“I am always surprised by the postnatal ward summary – it normally goes something like this: on the postnatal ward we have 70 mothers, 40 of whom have their babies with them. My immediate thought is – what happened to the other 30 babies?”
Dr Soha Sobhy is an Obs & Gynae doctor from London who has taken a year out of her specialist medical training to volunteer in Malawi with Ammalife. Soha shares her new experiences, the challenges she faces and raises awareness about global maternal health issues in her news:
Every morning we have a handover where the last 24 hrs statistics are reviewed for every ward and special cases discussed both as a learning point and also to help in patient management. I am always surprised by the postnatal ward summary – it normally goes something like this: on the postnatal ward we have 70 mothers 40 of whom have their babies with them. My immediate thought is – what happened to the other 30 babies? They go on to say 15 babies are in the nursery/neo-natal intensive care unit, and run through the statistics e.g 3 for birth asphyxia, 4 for prematurity etc. but there is still always a percentage unaccounted for. These are the babies that have died – fresh still birth, macerated still birth and early neonatal deaths and it’s easy to see why these occur.
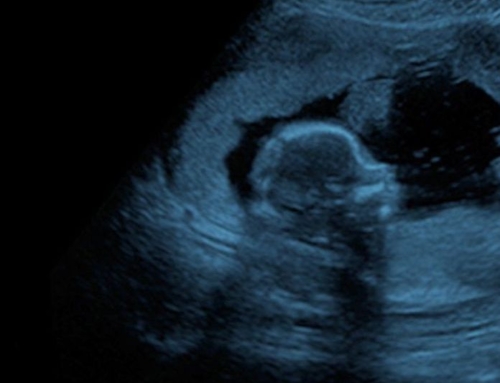
It is too late to do anything about the macerated still births once they reach the hospital. The mum arrives and already there is no fetal heartbeat detectable and hasn’t been for a few days. Sometimes this is because of the distance the woman has to travel to reach the health facility. It’s sometimes due to poor patient education and the women not knowing to be vigilant for changes in fetal movements which could indicate problems. Sometimes, it’s the lack of antenatal care so early problems aren’t detected and addressed.
The bigger problem however and one that we can do something about are those babies who die within labour. Imagine carrying your baby for 9 months, coming to hospital, going through a long labour only to deliver a stillborn baby and be told that your baby has died – it must be heartbreaking! The guidelines are that the fetal heart should be listened to every 30 minutes in the first stage of labour and every 15 minutes in the second stage of labour. This is just not feasible with the large patient load and staff shortages and sometimes the fetal heart is only listened to once or twice in labour, and so fetal distress is missed and poor outcomes are common.





Leave A Comment